Why admitting Covid is Airborne is so hard.
Evidence for airborne spread of Covid-19 is strong, but authorities underemphasize airborne protections. The curious history of infectious disease reveals how this anti-airborne bias emerged.
The evidence is strong that Covid spreads through the air, but neither the CDC nor the WHO will explicitly say so.
The evidence that Covid-19 spreads through the air has been there since early in the pandemic - in a Seattle choir, a Chinese restaurant, an Arkansas prison. And “Covid is Airborne” scientists have from around the globe who specialize in airborne contaminants have been pleading with authorities to tell the world, holding symposiums and writing editorial after editorial.
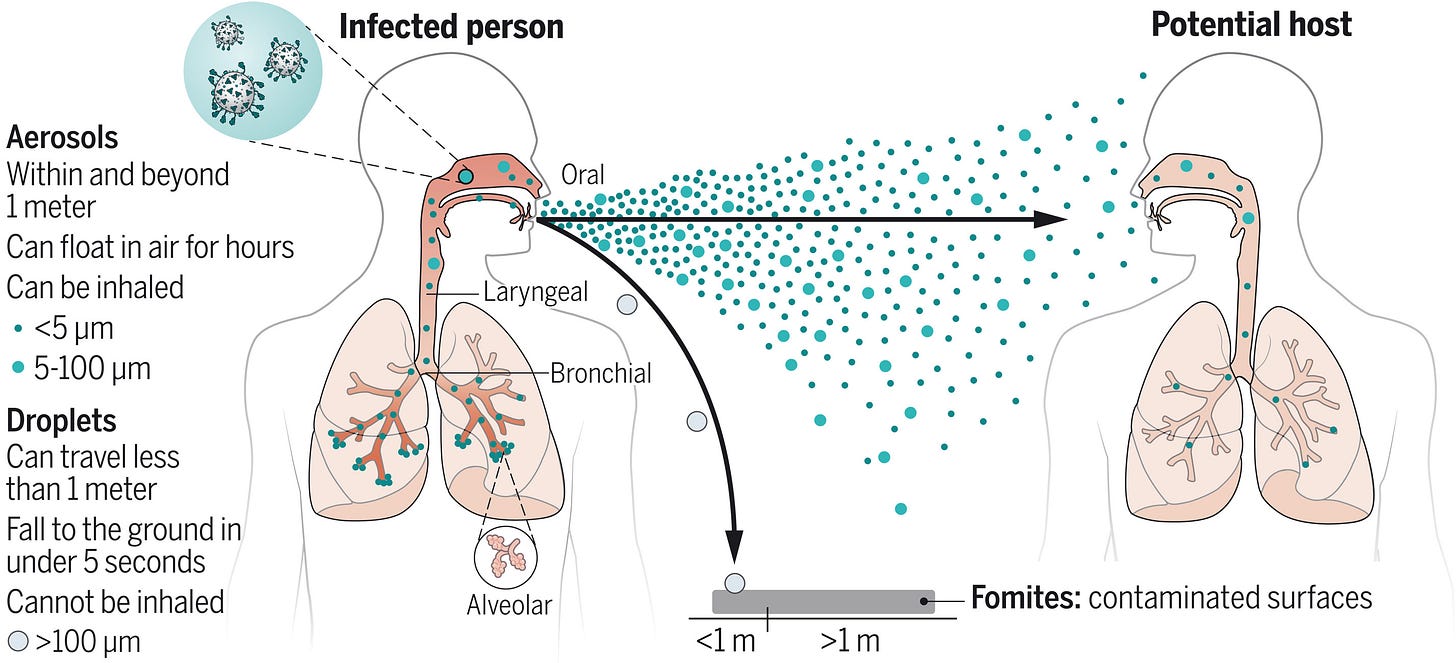
Virus-laden aerosols (<100 I1/4m) are first generated by an infected individual through expiratory activities, through which they are exhaled and transported in the environment. They may be inhaled by a potential host to initiate a new infection, provided that they remain infectious. In contrast to droplets (>100 I1/4m), aerosols can linger in air for hours and travel beyond 1 to 2 m from the infected individual who exhales them, causing new infections at both short and long ranges. CREDIT: N. CARY/SCIENCE
These aerosol experts have published studies on mask efficacy, how droplets of various sizes behave, and how air cleaners could trap the respiratory aerosols . They wrote an open letter in June of 2020 signed by hundreds of fellow scientists appealing to “national and international bodies to recognize the potential for airborne spread” of COVID-19. They have shown that 85% of viral load is in the air. They have explicitly laid out how respiratory viruses hitchhike on aerosols to penetrate the lungs and infect people.
And yet despite all this, and even as the Delta wave - as contagious as (the known-to-be-airborne) chickenpox - rages, there has been no clear guidance from the most prominent public health authorities that Covid is indeed airborne, in plain language that regular people and businesses can use to modify their own behavior and prevent airborne transmission.
Why can’t they just say “Covid is Airborne?”
The basic answer is simple: the reason authorities aren’t saying that Covid is Airborne is there is a strong bias against believing it to be true. That is, the public health and epidemiological literature almost uniformly says that airborne transmission is rare, so it’s very hard to believe that it’s actually happening at scale.
For virtually every disease you can think of, the guidance is that close contact with “respiratory droplets” and fomites - and not the air - are how infectious diseases transmit.
Take Mumps for example. The European CDC says it spreads via aerosols (and respiratory droplets), but the guidance from the CDC is still based on the idea that ballistic droplets and surfaces are the key mode.
Sound familiar? It’s the same default advice for Covid. It’s almost the exact same advice for flu (another airborne respiratory virus).
This contact-and-surfaces notion appears to be hardwired into any disease response, because as you will see, a contact and fluids approach has been incredibly effective at controlling disease and improving public health.
In fact, the discovery of contact infection and germ theory was a revolution, and the stories that led to that revolution are both interesting and point to the difficulty in overcome scientific biases once a community of peers has adopted a common view.
To understand the bias against airborne transmission, we need to go back to cholera.
To understand the Covid-is-airborne reluctance, we need to understand history as public health experts do, for the world-changing history of contact transmission informs the work they do today. And there is perhaps no more famous story in the realm of infectious disease (and the long history of airborne transmission) than the discovery of how cholera spread, so we will start our history lesson there.
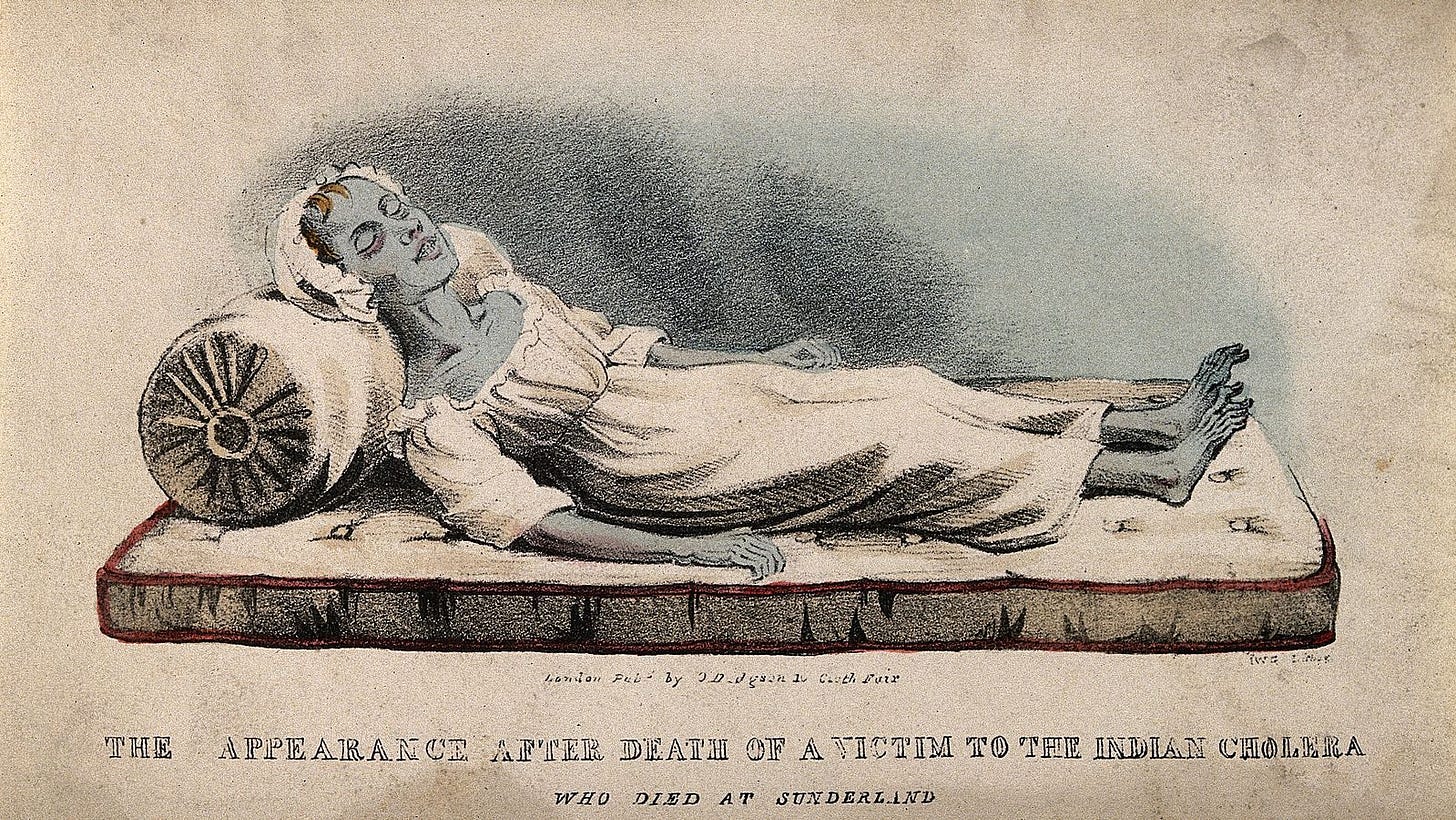
In the early 1850s, the third cholera pandemic was ravaging the world.
Two earlier cholera pandemics in preceding decades had killed millions, but in the nascently industrial late 1840s, global trade networks expanded, and the disease spread more easily to new places. And where it arrived, it brought suffering.
If you contracted cholera, you could lose five gallons, or to put it in a more relatable unit, forty pounds, of fluids in a day through uncontrollable “rice water” diarrhea and vomiting. “Rapid dehydration left its victims drawn…hollow…discolored…and hauntingly blue.”
With early intervention, cholera was treatable with commonly available castor oil or opiates, but once symptoms worsened, cholera could kill about half those who got it, sometimes within hours. Other diseases killed more in the nineteenth century, most notably tuberculosis - “consumption” if you remember your Dostoyevsky - but the way that cholera just drained its victims of fluids until their blood was too thick to flow made it uniquely horrifying.
The trouble was that to catch it early victims needed to act when symptoms of intestinal distress were mild. But the conditions in which most 19th century city-dwellers lived made such symptoms quite common and thus easily ignored.
Urban life in the mid-19th century was almost unspeakably filthy.
This was especially true for the poor. Masses of residents lived in tenement housing, almost always overcrowded and frequently lacking running water and sanitation. People bathed infrequently, had just a few changes of clothes, and dumped their trash and solid waste into the streets or private cesspools that festered in the sun and overflowed in the rain. The most unpleasant smells you can imagine would have been thick, ubiquitous, and unavoidable.
Life expectancy at birth at the time was in the mid-40s. More than 20% of infants died within a year of birth.
In 1849, a letter from a group of London’s poor was published in The Times, describing their plight: “We live in muck and filth…we got no..dust bins, no drains, no water splies, and no drain or suer in the hole place...we all of us suffer…if the colera comes, Lord help us.”
We didn’t know how cholera spread, so we made bad decisions.
In these conditions, cholera outbreaks spread quickly and killed relentlessly. Making matters worse, the authorities were convinced the disease spread through bad air, what was known then as “miasma.”
This, as we will see, was totally wrong, and thus misguided the response of public health authorities to prevent transmission. Consequently the death tolls that many cities suffered during the third cholera pandemic were high. Almost hard to believe.
Cholera outbreaks were incredibly deadly.
In 1849, New Orleans suffered the loss of 7% of its population to cholera - nearly 20 times greater than the total mortality that New York City has suffered from COVID-19.
St. Louis, despite advance warning of the woes downriver, lost “at least six percent of its population” to cholera the same year. Two waves of cholera hit Chicago a few years later and killed “at least 1,400,” or nearly five percent, of the city’s 30,000 residents.
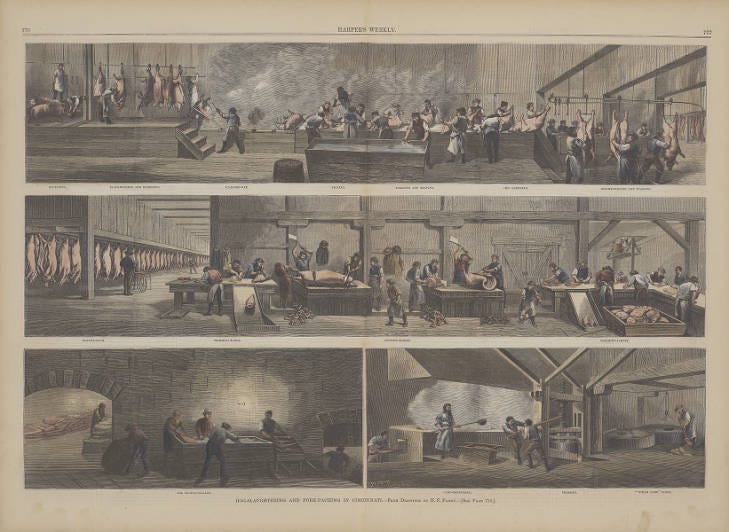
Cincinnati, a river city with no sewer system and a hog slaughtering industry so large people called it “Porkopolis,” lost 8,000 to the 1849 wave. Nashville lost six percent of its population, and was notable in that among its dead was recently departed President, James K. Polk.
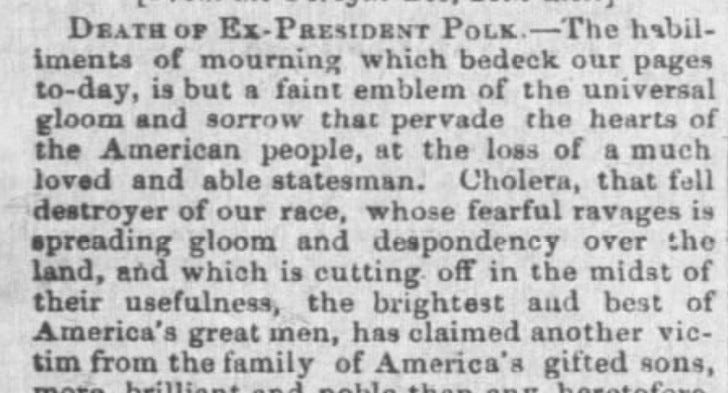
Since he had left office just a few months earlier, you might expect that Polk would have received a state funeral as a symbol of national pandemic loss, but after succumbing to cholera in June of 1849, the former President was put in a mass grave with his fellow victims.
Not even a President’s body was worth the risk of further spread through miasma.
Why? Because miasma was associated with corpses and rot, and “laws meant to prevent infectious diseases spreading from corpses” required it.
The devastation brought on by cholera felt not like a tractable problem, but instead like some supernatural punishment. Days after Polk’s death, President Zachary Taylor declared the need for a National day of “fasting, humiliation, and prayer” to address the “fearful pestilence...spreading its ravages throughout the land.”
He called on businesses to close, and for everyone to “acknowledge past transgressions” requesting that August 1st, Americans should “refrain...from secular occupation” to ask God to “stay the destroying hand now lifted up against us.”
Surrounded as so many were by stench, disease, and suffering, the belief that corrupt air spread disease is perhaps understandable.
Bad air was always thought to be the cause of disease.
We had also believed that the air spread disease for a very long time. Hippocrates, the “father of medicine,” wrote more than two thousand years earlier that “whenever many men are attacked by one disease at the same time, the cause...is which we breathe in.”
When cholera struck, it was assumed it spread through miasma because bad air was the default explanation for any diseases that a lot of people got at once. Malaria for example, which everyone knows now is spread by mosquitoes, was literally named after a colloquial Italian word for bad air - mal-aria.
The Plague too was thought to spread through the air. You have probably seen the haunting, bird-beaked plague masks in pop culture images before. These were not designed to terrify (though they are quite creepy) but instead to force respiration through scented herbs like lavender to prevent the foul air thought to carry plague from reaching physicians.
Given the strength of these traditions and given that the quality of air was terrible wherever cholera outbreaks occurred, few questioned that the air was the culprit.
But one person believed cholera didn’t spread through the air.
About the same time President Polk was dropped into a mass grave in 1849, an obstetrician in London named John Snow argued in “On the Mode of Communication of Cholera” that the disease spread not through putrid air, but instead through water. Specifically, Snow wrote that it spread “by the emptying of the sewers into the drinking water of the community.”
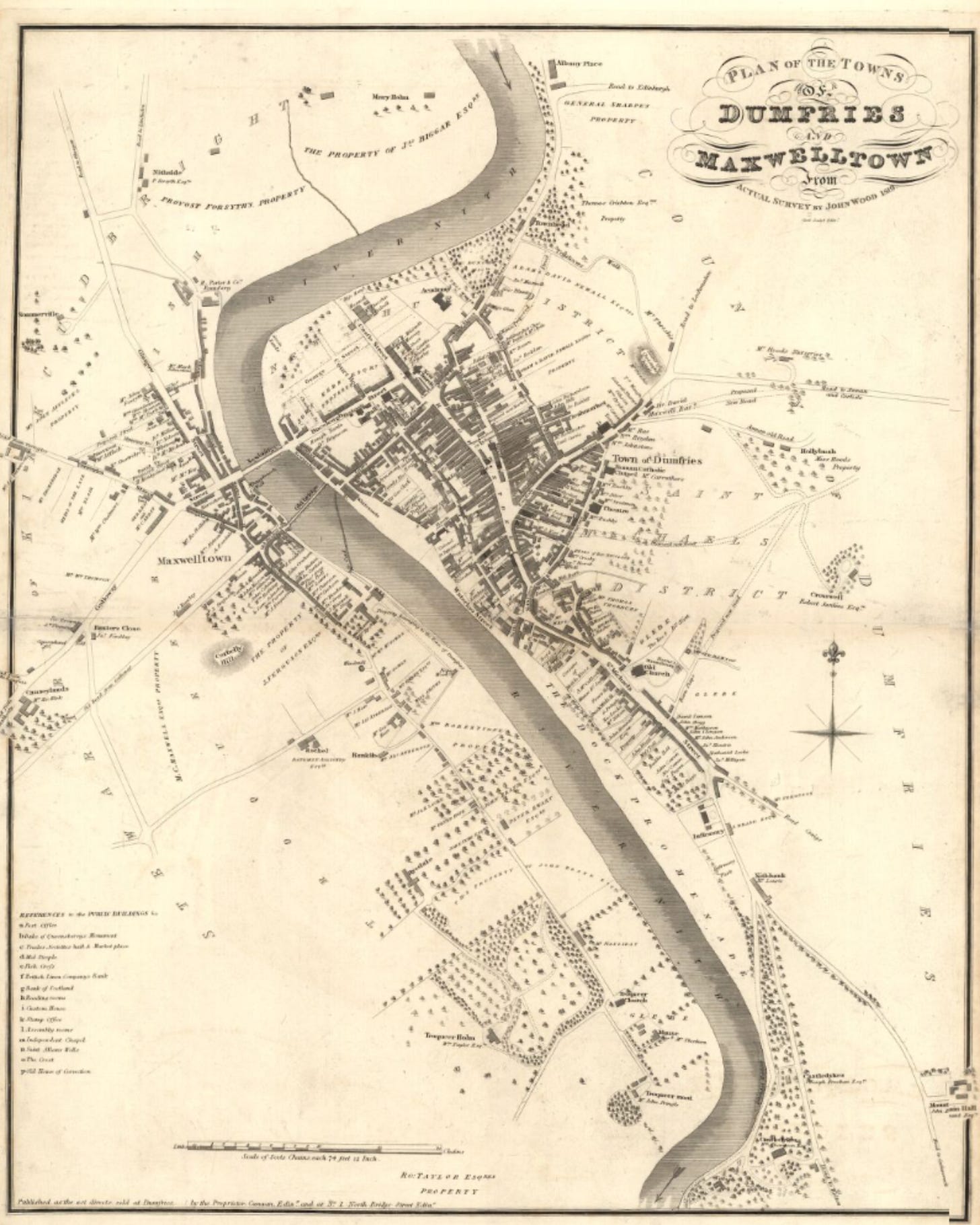
In one account, Snow describes the twin Scottish towns of Dumfries and Maxwelltown, which had lost around 3% of their combined population as “not usually an unhealthy place,” but then notes that their “inhabitants drink the water of the Nith, a river into which the sewers empty themselves, their contents floating afterwards to and fro with the tide.”
Reading his work with the knowledge we have now, it’s puzzling that it took so long for people to listen to him. Snow’s career would be defined by trying, but mostly failing to convince others to change their minds about miasma and cholera.
John Snow’s evidence pointed to water. But even good evidence was ignored.
He knew his waterborne theory was inconsistent with the miasmatic consensus, but his observations pointed to contaminated water. He had meticulously documented the geography of local outbreaks over decades of previous cholera pandemics in England.
He had studied exactly which districts of London took their water supply from the sewage-filled Lea and Thames rivers and noted that cholera was more prevalent there than “other parts of the metropolis, differently supplied.” He had studied how the tidal flows of the Clyde river unavoidably pushed waste back into the water supply of Glasgow, a city which had lost thousands of citizens to “the malady.”
Even as Snow became convinced in 1848 that he was right, he considered his existing evidence “so scattered and general a nature as to not make a ready and easy impression.” Snow had thus hesitated to publish his 1849 article until he had more “direct proof.” This he thought he found, but despite the detailed, down-to-the-street level evidence he provided, Snow made no headway in convincing London’s public health authorities to change their minds, even as outbreaks continued to flare up.
Snow disabled a pump to prove this theory. It worked. But it wasn’t enough.
Another such outbreak struck London in 1854, this time in Soho, which had recently become a densely populated neighborhood housing many garment workers for Regent Street shops. This specific outbreak was devastating, killing some 500 neighborhood residents in a single week. Snow drafted a detailed map of deaths, marking the locations of neighborhood water pumps.
He noted the roughly radial concentration of deaths surrounding the Broad Street pump, and that the nearby Brewery and Workhouse, both of which had their own water supplies, saw far less mortality. He concluded that the Broad Street pump itself was the source of the outbreak.
This time, he “persuaded the doubtful civic authorities to remove the handle from the Broad Street pump, and the already subsiding epidemic disappeared within a few days.”
Snow became a hero for his work, but he never knew it.
As a result of his discovery, Snow and his map later achieved legendary status in public health circles. The Broad Street Pump itself is now a monument.
But John Snow never knew his work was celebrated. Despite his success in Soho, his conclusions were nonetheless again rejected by the health establishment.
The tidily named Scientific Committee for Scientific Enquiries in Relation to the Cholera Epidemic of 1854, headed by William Farr, reviewed Snow’s Broad Street data and wrote that it did “not feel it established that the water was contaminated in the manner alleged,” and saw “no reason to adopt this belief” that cholera was borne not by air but water.
Nevertheless, in response to public outcry to do something, the miasmatists in charge began to push for large-scale sanitation measures that included among other things a focus on the “purity of the water supply.”
Even as Snow’s work led authorities to deploy some changes his theory suggested, they did so by adding new precautionary procedures related to the water while still holding to the miasmatic view rather than examining all the implications of a new theory.
Snow would be dead for eight years before his chief critic on the Broad Street matter, William Farr, eventually admitted the correctness of Snow’s waterborne theory in 1866.
Fortunately, the measures undertaken to improve the water supply greatly reduced mortality from subsequent cholera outbreaks. Glasgow, which saw nearly 4,000 die of cholera in 1854, lost just 68 when it returned in 1866 after moving the source of drinking water to an uncontaminated lake. Though the miasmatists were slow to recognize the failures of their theory, such evidence that they were wrong would continue to build to inform the work of the next generation.
Even though miasma failed, it persisted to be blamed for many maladies.
Just as in the present we have learned that diseases once thought to be spread by surfaces and droplet contact are actually primarily aerosol, there were other scourges in the 19th century that were falsely attributed to miasma.
Medical infections were responsible for millions of deaths too. Like cholera, the cause of such infections was generally thought to be the bad air. The world would soon experience the incredible, life-extending power of antiseptic procedures - washing hands and surfaces - but as with cholera it would acknowledge the need to change only very reluctantly.
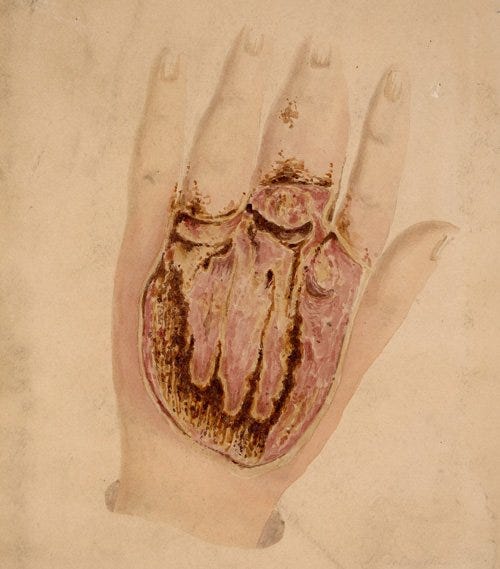
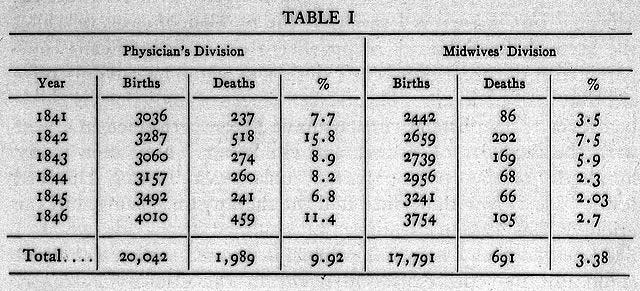
Hungarian doctor Ignaz Semmelweis observed in 1847 that mothers who delivered with doctors and residents had mortality rates five to six times higher than those who delivered with midwives. They weren’t dying during childbirth, but instead became sick a few days after and succumbed to fever and severe abdominal pain. After studying the matter, Semmelweis realized that the doctors regularly handled corpses just before delivering babies, while the midwives did not.
His solution was to require that doctors wash their hands in a chlorine solution before births. After this intervention, maternal mortality from “Childbed Fever” fell from 10% or more to 2%. It fell further to 1% when he required that surgical instruments be washed as well. His insight yielded a 90% plus reduction in maternal deaths. Childbed Fever was second only to tuberculosis at the time in causing death among young women, so this was a world-changing innovation that would ultimately save millions of lives.
Though hand-washing reduced mortality, miasmatists credited clean air.
But his superior, a dedicated miasmatist professor named Johann Klein, didn’t accept Semmelweis’ conclusions, despite the improvements.
Klein, believing that the air itself was the problem, attributed the change not to hand washing, but to the facility’s new ventilation system, which had helped to clear miasma.
Amid this disagreement, and perhaps because of it, Semmelweis lost his assistant professorship in 1849. After spending the next dozen or so years trying to convince others of the power of sanitary procedures, Semmelweis died at the age of 47 in an insane asylum. He had been beaten by guards, and it is speculated that he himself died of an infection that resulted from the beating. Like Snow, Semmelweis died never knowing the eventual impact of his work.
Miasma was thought to cause infections in amputees too.
Doctor Joseph Lister enjoyed a similarly inhospitable environment in England for his research. In the 1860s, amputations had become more bearable due to the introduction of anesthesia, but around half of amputees were still dying in post-op recovery.
Across Europe, the solution at the time was to increase space between patients to “limit miasmatic transmissions” and make smaller incisions when possible so as to reduce the area exposed to “atmospheric poisons.” Lister, influenced by Louis Pasteur and early suppositions about microorganisms, experimented with the soaking of wound dressings in carbolic acid, which though unpleasant, acted as an antiseptic.
Lister’s experiments yielded dramatic drops in mortality, but he struggled to convince others. There were several problems. First, his methods took time and effort on the part of physicians. Second, these efforts seemed pointless as they were inconsistent with miasmatic theory. To one who believed in miasma, Lister’s arguments weren’t just unconvincing, they were irrelevant. As a summary of Lister’s career in the Lancet puts it, “If one did not believe bacteria caused wound infections, then adopting a method to eradicate bacteria made little sense.”
Lister suffered a happier fate than Snow or Semmelweis. You may not have heard of Joseph Lister before, but you have almost certainly used the popular mouthwash named in his honor.
As with cholera though, it took too long for good work to be understood.
Only decades after Semmelweis’ death and Lister’s initial publications did the significance of their work become clear. Over time, plenty of evidence had been building that contact and fluids were responsible for many of the most unpleasant and tragic ailments once blamed on the air, but as Max Planck suggested,
“A new scientific truth does not triumph by convincing its opponents…but rather because its opponents eventually die, and a new generation grows up that is familiar with it.”
But change was coming.
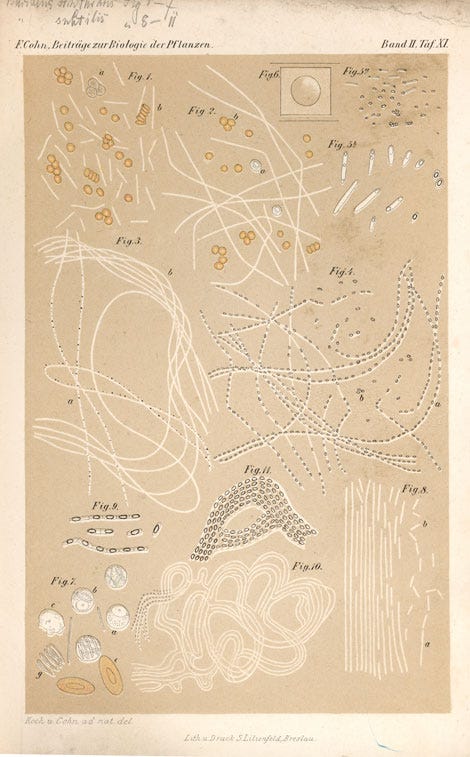
In 1875, the notion that tiny organisms were responsible for the spread of disease - germ theory as it came to be known - was gaining broader acceptance among a new generation of scientists. But no one had isolated a specific example of such an organism until Robert Koch did so with the bacterium that causes anthrax.
Influenced by both Lister’s and Pasteur’s work, Koch set to investigating a local anthrax outbreak that had killed hundreds of people and tens of thousands of livestock. Through innovative work in culturing the “rods” he observed in blood samples and much experimentation, Koch was able to prove that this bacteria was responsible for the disease.
He furthermore explained how contact with contaminated soil even years after an outbreak could act as a source of future outbreaks. This discovery was, in essence, the missing link.
The notion of contagion had been around for a while, but it lacked proof. Finally here was a mechanism - contact with actual organisms - to point to. Once scientists realized what they were looking for, they found more germs. Within a decade of Koch’s discovery, “German microbiologists isolated the organisms that cause cholera, typhoid fever, diphtheria, pneumonia, tetanus, meningitis, gonorrhea, as well the staphylococcus and streptococcus organisms.”
Why was miasma theory so durable? Because science often resists change.
With a new, observable mechanism in place, and one that allowed for dramatic public health improvements through policy interventions, germ theory took hold. Even so, belief in miasma had endured for decades longer than it should have, despite all the evidence that is plain to us now and despite all the grinding, thankless work by dedicated scientists.
As the history of science has shown though, the delay in adopting a new paradigm has been the norm in science, and the lessons of the past are a helpful warning to those inclined to resist change today.
Thomas Kuhn, author of The Structure of Scientific Revolutions, writes that resistance to change is actually a part of the critical functioning of “normal science.” Normal science is a “cumulative enterprise” that relies on a basic agreement about what it is that scientists are working on. Without this commitment to a common foundation, scientists can’t collaborate across time and space.
Most of the time, this resistance is helpful.
Kuhn writes that
“normal science often suppresses fundamental novelties because they are necessarily subversive of its basic commitments.”
Normal science is thus essentially conservative, especially when it comes to fundamental operating assumptions. It wouldn’t work otherwise. Conservatism is a feature, not a bug, as it helps preserve collective focus from distraction.
When the operating assumptions are wrong, as they were with miasma, anomalies and inconsistencies thus initially get suppressed by the collective pressure of normal science. This is why the research of Snow, Semmelweiz, and Lister encountered resistance - all of their work went against the operating consensus. Their work started a revolution in science, but it did so in slow motion.
Revolutionary science often meets fierce resistance, delaying progress.
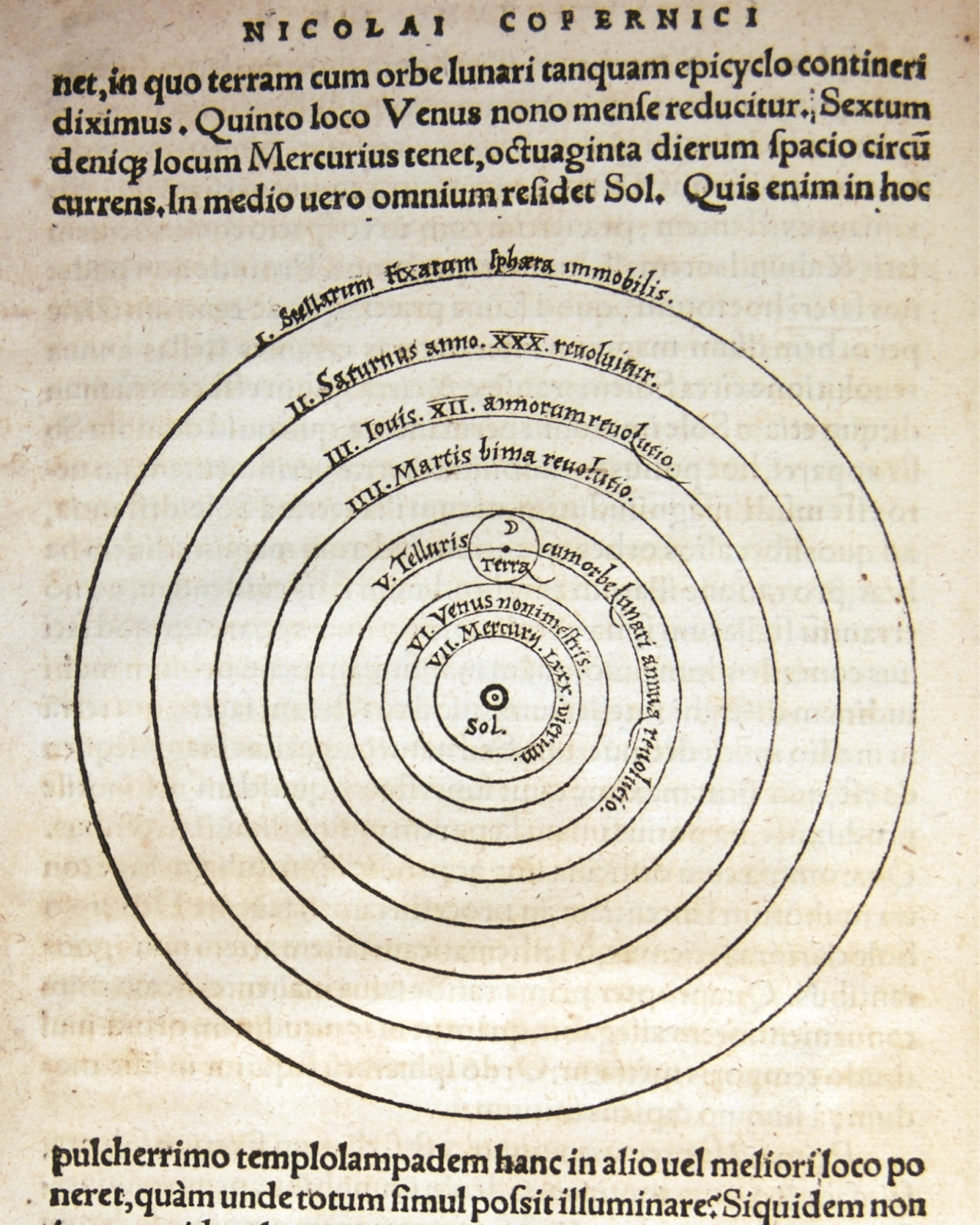
This is because revolutions in science are “tradition-shattering.” The Copernican Revolution, the theory of evolution, special relativity - they all encountered serious resistance en route to adoption because like germ theory, they rewrote fundamental assumptions.
When a revolution is finally achieved, the old theory is thrown out.
But despite resistance, these revolutionary ideas are inexorable. Such was the case with germ theory. It took decades to complete, but once germ theory finally took hold it wouldn’t just be added to the idea that air carried disease, it would create a new foundation of understanding for all scientists who came after.
The foundational belief that the air carried disease was effectively abandoned and replaced by the understanding that germs did.
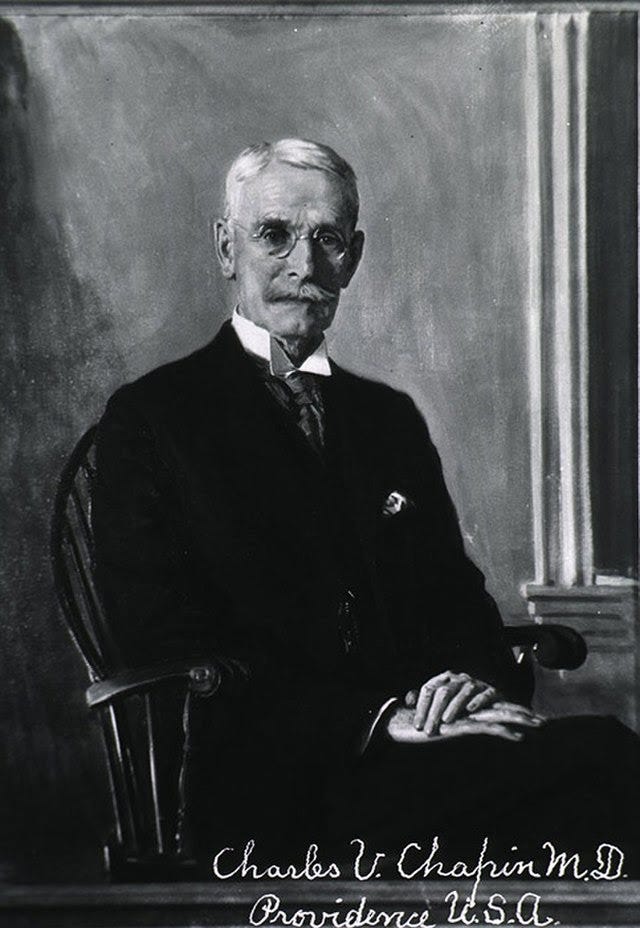
In 1910, Charles Chapin helped finalize this replacement when he published The Sources and Modes of Infection, a seminal work in which he systematically argues that infections are spread by close contact, when one person spreads germs - bacteria, parasites, and the like - to another through direct contact.
Unlike the superstitious miasma theory of old, contact transmission was supported by real evidence - organisms that could be observed and cultured from surfaces. Chapin even cites Snow’s work - he was effectively describing contact transmission before it had a name - among many documented examples of historical contact transmission that weren’t then recognized as such. And Chapin saw little reason to consider airborne transmission at all given what we now knew.
Thus, belief in airborne transmission was discarded in favor of germ theory.
Chapin writes of airborne spread, “...without denying the possibility of such infection, it may be fairly affirmed that there is no evidence that it is an appreciable factor in...our common contagious diseases. We are warranted, then, in discarding it...and devoting our chief attention to the prevention of contact infection. It will be a great relief to most persons to be freed from the specter of infected air, a specter which has pursued the race from the time of Hippocrates…”
Note two things. First, Chapin is motivated in part out of a worry that people will avoid contact protections if they believe a disease spreads through the air. Many have speculated that this has been a part of our current reluctance too.
Second, the use of the the word “discard” here shows where we abandoned it. The airborne theory of disease transmission, which had been the dominant view for two thousand years, was being thrown out because the real cause of disease had been found.
Chapin’s dismissive characterization of airborne transmission was tied to the then recent superstitious history of miasma and his fear of losing hard-earned progress of contact mitigation, but the attitude and tone he took toward aerosols has propagated through infectious disease literature ever since he published. Indeed, his words are echoed in this pandemic 110 years later.
Chapin’s dismissal of airborne transmission still lives on.
In July of 2020, JAMA published an article entitled Airborne Transmission of SARS-CoV-2, Theoretical Considerations and Available Evidence, in which the authors write “notwithstanding...the possibility of aerosol-based transmission, the data on infection rates and transmissions in populations...are difficult to reconcile with long-range aerosol-based transmission.”
It’s the same basic language that Chapin had employed.
In many ways what is happening here is similar to what happened in the cholera pandemic in 1855. We have a theory which has been dominant for some time, and we see public health authorities resisting changes to that theory despite the fact that new science from outsiders offers a better explanation of how a pandemic disease is spreading.
The trouble is that “droplets” don’t drop.
Two days after the JAMA article’s publication, an aerosol chemist from CU Boulder named Jose-Luis Jimenez took issue with the authors’ definition of droplets, which they defined as “larger entities (>5 μm) that rapidly drop to the ground by force of gravity, typically within 3 to 6 feet of the source person.”
Droplets, by this definition and by the CDC’s advisory committee, were in effect, contact transmission, delivered ballistically from one person to another. This definition gave us plexiglass barriers and face shields. This definition is what’s behind keeping six feet of distance, safely outside the ballistic range of another person’s respiratory droplets.
But, as Jimenez noted, to suggest that 5 µm particles “rapidly drop” requires the physics of another planet.
“For particles of 5 µm to fall...quickly, gravity on Earth would have to be 100 times larger than it is,” Jimenez wrote in response to the article.
To a professor who had spent his life studying the movement of particles through the air, this was like reading that the disease spread through feathers but that these feathers acted like marbles. This was a misunderstanding of the basic physics of small particles.
Other specialists in aerosols had also noted this error. In April of 2020, as detailed in the excellent Wired piece, Linsey Marr, an environmental engineer at Virginia Tech, and Lidia Morawska, an atmospheric physicist, were able to connect via video chat with the WHO.
Morawska “tried to explain how far infectious particles of different sizes could potentially travel. One of the WHO experts abruptly cut her off, telling her she was wrong.”
Contact tracing showed that people within ballistic range of coughs most often contracted the disease, so droplets explained it.
Aerosols are concentrated at the source, so more transmission should be close.
But Marr explained later in the New York Times that that was because aerosols are like cigarette smoke - they have much higher concentration at the point of emission. You would expect then, that transmission rates would be higher closer to the source. This should have been seen as evidence for aerosols, but instead of preparing for a winter of open windows, the pandemic continued without official word that aerosols played a major role in transmission.


Later in the Summer, Marr and atmospheric chemist Kimberly Prather presented summary information to Dr. Anthony Fauci, explaining the foundational mistake about the behavior of droplets in the medical literature. To Fauci’s credit, in an interview shortly after that presentation, he acknowledged that “we are learning” and admitted a “degree of aerosolization.”
Over the fall and winter, momentum slowly built to support the aerosol theory. More superspreading events emerged and it became clear just how much transmission was happening in indoor, low-ventilation environments and how little appeared to be happening at beaches, parks, and protests. But the official guidance at the CDC and WHO hadn’t changed, which meant that many were still acting as if six feet or plexiglass acted as an effective barrier to transmission.
Here is where the story gets a bit more hopeful.
During the time of miasma, those arguing against it mostly toiled in isolation, unable on their own to push back against the tide of consensus. This was not the case today. Hundreds of prominent scientists had come together. They were able to identify some central semantic problems - how droplets were misnamed, how aerosols meant one thing to physicists and another to physicians, how the word airborne itself was loaded - and they had been compiling their evidence in a common language of science that they believed would be understood by the medical and public health communities.
On April 15th, famed medical journal The Lancet published Ten scientific reasons in support of airborne transmission of SARS-CoV-2. The paper systematically presents the evidence that airborne transmission of Covid is “likely to be dominant,” suggesting that “the public health community should act accordingly and without further delay.” Among its other arguments, the article notes that
“…diseases once considered to be spread by droplets are airborne.”
The same mistakes about droplet and aerosol behavior that presented with SARS-CoV-2 have been made with many other diseases.
The implication here is that it’s not just Covid. This is happening with other diseases because our response to other diseases is based on the same understanding of close contact. That’s why the ballistic-droplet-and-surface advice to limit transmission is the same.
Our misnomered view of aerosol spread limits the evidence we look for.
Just as miasma theory influenced what evidence was admissible to miasmatists, the consensus understanding of the nature of close contact transmission perpetuates the misunderstanding of aerosols - if you believe that airborne spread is unlikely it will limit where you think to look for evidence. And this belief will influence how you interpret the evidence you find. In this excellent review of aerosol transmission, the authors note that
“…despite the various mechanistic arguments about which organisms can be potentially airborne and therefore aerosol-transmissible, ultimately, the main deciding factor appears to be how many studies using various differing approaches…reach the same consensus opinion…”
If we examine the WHO’s early all-caps declaration that, “FACT: #COVID19 is NOT airborne” we see the problem.

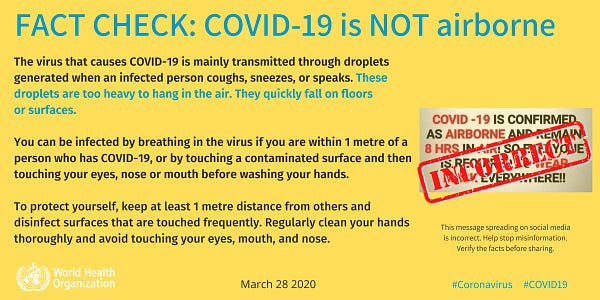
The statement was not based on emerging evidence from SARS-CoV-2, which even then suggested aerosol spread, but instead on the convention that diseases don’t usually don’t spread through the air.
But the convention that other diseases spread primarily via surface and contact is based on the same misunderstanding of aerosols that led us astray with Covid-19.
This is not to say that all diseases spread via aerosols or that hand washing and sanitation are not important. You have just read multiple examples of maladies wrongly attributed to airborne spread and learned that millions of women likely died for lack of basic hygiene.
We are STILL missing the bigger story. It is not just Covid.
Even as journalists highlight how we were wrong about Covid-19 and aerosols, the broader point is being missed, which is why the convention on which the WHO relied is so insidious. The Economist piece about ventilation suggests that advice about hand washing and surfaces for Covid “makes sense if SARS-CoV-2 spreads in the same way as influenza.” But they do, or at least can, spread the same way - through the air.
The new physical understanding of aerosol transmission should mark a paradigm shift.
We have observed the many parallels between the cholera and covid pandemics, and we observe another here.
Before cholera we thought that some corruption of the air itself spread disease. Obviously, the miasmatists were wrong. There is in fact no such thing as miasma. It was germs…like Chapin said, passed from one person to another all along. And while these germs can spread in a variety of ways - most diseases are probably multi-modal - it’s clear that the medical literature developed a blind spot to the extent of airborne transmission.
And now we are learning that other diseases we have thought to be spread via “droplets” and fomites almost certainly spread primarily via aerosols. Indeed a recent paper in Science says “there is robust evidence supporting the airborne transmission of many respiratory viruses, including severe acute respiratory syndrome coronavirus (SARS-CoV), Middle East respiratory syndrome (MERS)–CoV, influenza virus, human rhinovirus, and respiratory syncytial virus (RSV).”
Given the history of airborne spread that public health officials know well, it seems as though the notion of airborne spread has been characterized negatively because it had already been discarded. As we emerged from the era of folk science, “society neglected and forgot aerial health practices when germ theory promised better disease control,” writes Dr. Melanie Kiechle, a historian at Virginia Tech.
The literature is right about contact with germs, but thanks to the urgency of this pandemic we have come to understand that germs themselves can travel readily through the air in ways we thought they generally didn’t. This is a really big deal.
This new aerosol understanding should be a true paradigm shift.
A new theory - near field aerosols - now explains the past evidence of disease in better way than the old theory. It replaces a past understanding. If what was assumed to be droplet and surface driven transmission for so many other diseases has actually been near field aerosols, then we must re-examine all of our default safety protocols. It changes how we interpret past research and the equipment we use in the research of the future.
If Kuhn is right about normal science, then our institutions will be tempted to narrow the scope of these aerosol behaviors to Covid-19. This would be a huge mistake.
If we don’t act on this new knowledge, we are making our past mistakes contagious.
We have to consider the larger implication here. The decades-long delays in changing our mind after past novel discoveries are like secondary infections in a transmission chain. They are avoidable if we act more quickly.
If we respond as we have to past paradigm shifts, we will perpetuate the undue consensus that aerosols do not contribute to the spread of most diseases. We’ll be more vulnerable to future pandemics and seasonal illnesses because we’ll often be fighting on the wrong front.
But if our institutions are brave enough to consider that more, or even most diseases have strong aerosol components, then like the scientists during the German golden age of germ discovery, we will doubtless discover more that do. Finding them and intervening as we did then would prompt another revolution in public health.
This is a generational opportunity for improvement.
For thousands of years, we drank dirty water. And for thousands of years people suffered from bacterial and parasitic infections that halved human lifespans and robbed humanity of productivity. Then cholera came at the same time we were developing governmental institutions that were in a position to make public health decisions.
We cleaned the water, we washed our hands, and the world was changed forever.
Today each of us breathes in a swimming pool of air every day, and few among us give much thought to what’s in the air. Like cholera, a waterborne pandemic, before it, perhaps the airborne nature of Covid-19 inspires our scientists and politicians to make similar efforts to clean the air of germs, irritants, and carcinogens. If we do so, we’ll bring the pandemic to a quicker end and make the whole world healthier in the process.
The sooner we embrace this opportunity the better.













Typo:
"Today each of us breathes in a swimming pool of air every day, and few among us give much though to what’s in the air."
though -> thought
Great article, but you left out Snow's single strongest piece of evidence. Any comparison of neighborhoods was still in principle at risk for being confounded by different atmospheres. In one neighborhood, however, houses supplied by two different water companies were mixed together on a very fine scale, almost like a random assignment. One company had a source upstream of sewage, the other downstream. You can fill in the rest.